With access to social media and information networks, patients with a spectrum of abilities, prejudices, and levels of understanding may gain access to research, clinical trials, and practically endless resources for information about illnesses, procedures, and symptoms. Patients, advocates, family members and laypersons are now able to navigate a world of information that was once solely the domain of the physician, specialist, or researcher.
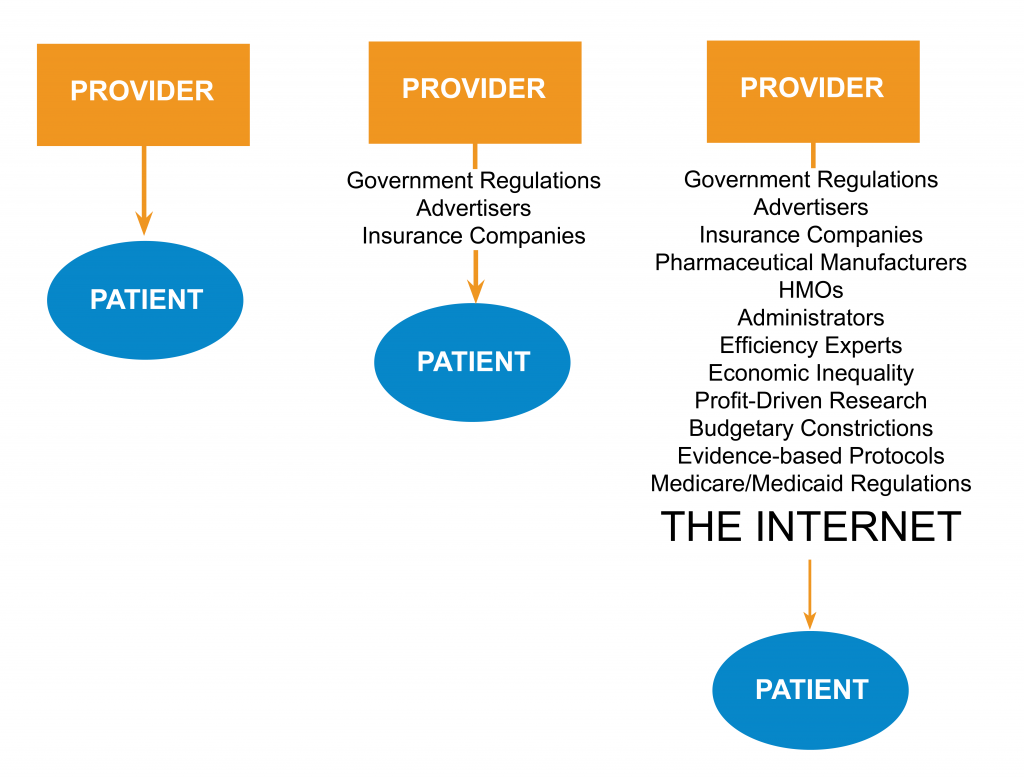
Provider-Patient Contact
Provider-Patient Collaboration
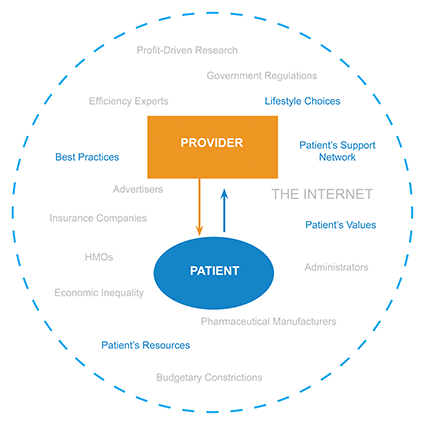
The principles of patient centered care are well-established and encouraged in mainstream institutions, so what makes this so challenging? Because even though we know best practices, established power dynamics in a hierarchical healthcare system are not conducive to these principles.
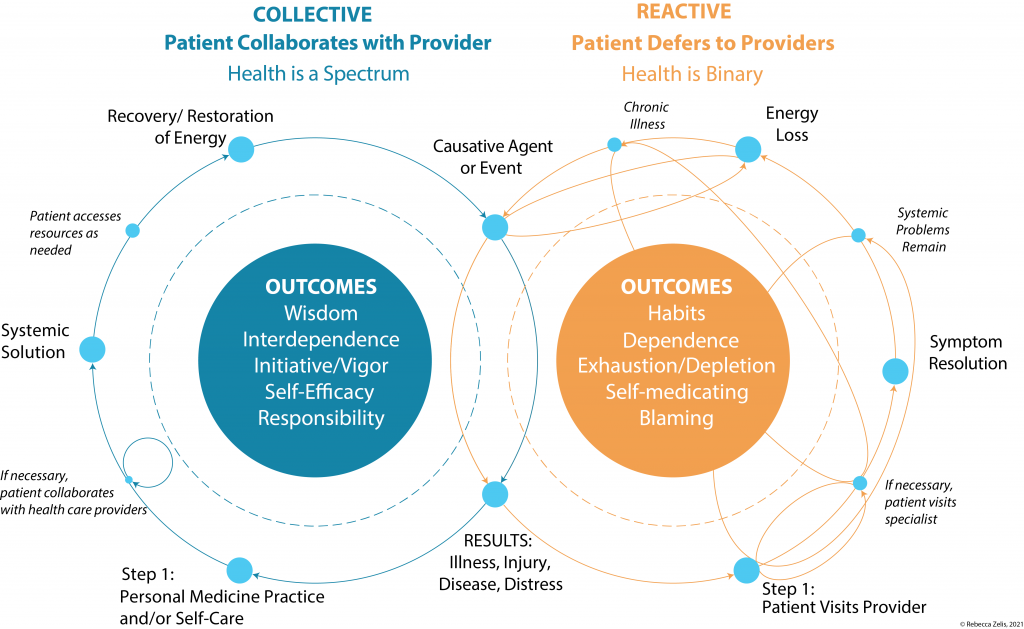
Events happen continually throughout a patient’s life that impact their health and well-being. The initial results are the the same in both cycles. The patient’s response decides if health care becomes a ‘Reactive’ cycle or a ‘Collaborative’ cycle. Reactivity increases dependency upon health care providers, resulting in ongoing, complex cycles that disempower the patient and increase the burden on providers. A focus on addressing symptoms neglects to address the etiology of a patient’s health problem(s) which is often multifaceted and systemic.
In a Collective approach decisions are not made in acute crisis, or solely for short-term symptom relief, but instead are proactive and aligned with the patient’s values, resources, and goals. The patient is empowered to implement lifestyle changes, practice self-care, and access preventative medicine. The result is heightened personal responsibility and restoration of energy, which builds resiliency and and prepares the patient for the next (inevitable) health challenge.
